Nutritional Psychiatry – Foods the Brain Needs for Success
The brain needs many foods for success; a lack of any one of the hundreds of nutrients will result in poor cognitive health and performance.
Anxiety disorders represent a significant and growing challenge in mental health, affecting a staggering one-third of individuals in the United States at some point in their lives.
Traditionally, these disorders have been addressed through drugs and therapies, yet these methods often fall short, effectively aiding only about half of those they treat.
This gap in treatment efficacy highlights an urgent need for alternative approaches. One such emerging field is metabolic medicine, an area of healthcare that delves into the intricate relationships between metabolism, diet, and disease management.
This article will shed light on the latest scientific advancements in using food and nutrition as tools to treat anxiety and other mental health disorders. It focuses on the profound impact our diet can have on our mental well-being, particularly through its influence on the gut microbiome and inflammation levels.
By exploring how certain nutrients and dietary patterns can either exacerbate or alleviate symptoms of anxiety, we offer insights into how you might better harness your diets as powerful allies in the war against anxiety.
As research continues to unravel the complex connections between what we eat and how we feel, it becomes increasingly clear that our approach to treating anxiety may indeed lie, at least in part, on our plates.
With such high failure rates from medication and the potential for side effects that are often worse than the symptoms they are trying to treat, we are likely treating neurological conditions with the wrong approach.
Anxiety and other mental illnesses have been shown to be metabolic diseases as much as they are psychological.
Neurological conditions like mental illnesses are characterized by fundamental metabolic disturbances, such as oxidative stress, insulin resistance, inflammation, and microbiome dysbiosis, to which lifestyle factors like our diet are a contributor. It makes sense, therefore, that mental illnesses deserve complementary lifestyle approaches.
The gut microbiome, a diverse collection of microorganisms living in the digestive tract, has gained significant attention recently due to advances in research revealing its crucial role in various aspects of human health, especially mental health. A whole new field has emerged from this microbiome-brain relationship: nutritional psychiatry.
Although not yet fully understood, the microbiome can induce anxiety by communicating to the brain via the Vagus nerves, where it regulates hormones and influences inflammation.
The specific composition of an individual’s gut microbial ecosystems can regulate mental status and anxiety, so it is unsurprising that microbiome dysbiosis (an imbalance in the normal microbial composition) is frequently associated with anxiety.
Research shows that mice raised in sterile environments, which lack a normal microbiome, have an enlarged and more active amygdala. Introducing specific beneficial bacteria to these mice, such as Bifidobacterium infantis, can normalize their stress responses, indicating the microbiome’s role in amygdala functioning.
The amygdala, which is involved in emotions like fear and anxiety, is affected by certain chemicals made in your gut. These chemicals, like NPY, PP, and GLP-1, can change how anxious you feel and are controlled by special substances called SCFAs, fatty acids made by good bacteria in the gut.
These SCFAs impact the release of gut peptides that regulate our stress response and anxiety levels via the amygdala, and people who often feel anxious tend to have fewer of these good bacteria that produce SCFAs.
The interaction between the gut and the brain is two-way; emotional stress can alter the gut microbiome through the release of stress hormones and neurotransmitters. Although current science may not allow for precision-targeted treatments based on the microbiome, understanding the complex interactions between our gut and brain is crucial in addressing anxiety disorders more efficiently and safely.

Chronic inflammation is a feature of almost all neurological and neurodegenerative disorders, including anxiety.
People with anxiety and related conditions, including panic disorder, generalized anxiety disorder, and PTSD, often have higher levels of inflammation-related substances in their blood and spinal fluid.
It is believed that cytokines, proteins released by cells to send signals to the brain, disrupt the balance of brain neurotransmitters like serotonin, dopamine, and glutamate/GABA, leading to increased activity in the amygdala.
The list of foods known to increase inflammation is extensive but generally includes foods associated with the Standard American Diet (ironically abbreviated to SAD).
In particular, refined sugars (candy, soda, and fast foods) and processed vegetable oils have both been shown to contribute to inflammation through various mechanisms.
Processed vegetable oils like corn and soybean, which are high in omega-6 fatty acids, particularly linoleic acid, can cause inflammation. These oils lack the antioxidants found in whole foods that normally protect omega-6 fats.
As a result, the linoleic acid in these oils integrates into cells and tissues, undergoes oxidation, and can start a harmful cycle of oxidation, insulin resistance, and inflammation. This cycle can contribute to metabolic and inflammatory diseases affecting various parts of the body, from the gut to the brain.
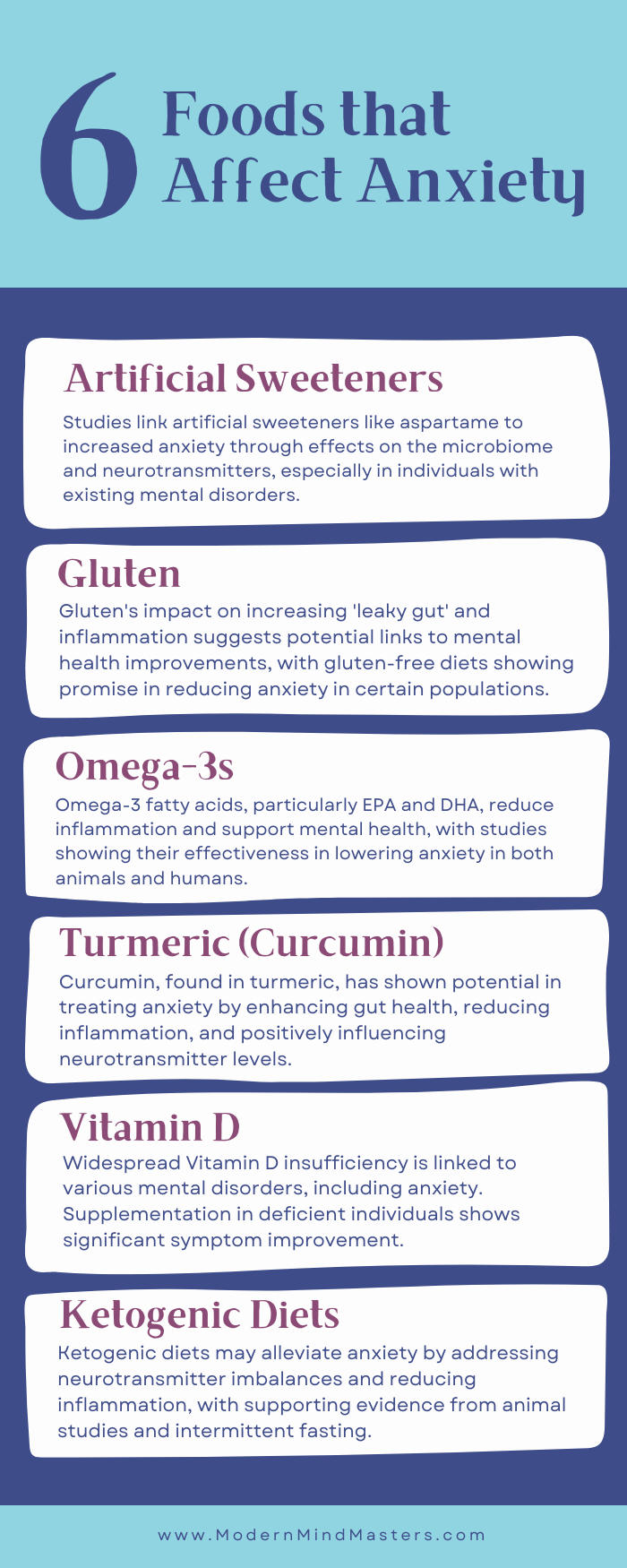
The link between artificial sweeteners, such as aspartame and sucralose, has been shown in animal studies to precipitate anxiety, and it is now thought that the anxiolytic (anti-anxiety) effects of such sweeteners are likely mediated by their adverse impacts on the microbiome and inflammation.
For example, this study gave aspartame to rats and found increased levels of stress hormones in the animals’ amygdalae.
Similar conclusions were reached for studies in humans, where aspartame was shown to block the transport of dopamine and serotonin precursors into the brain, shifting it toward a state prone to anxiety.
This crossover study unintentionally found that individuals suffering from mental disorders may be particularly susceptible to the adverse effects of artificial sweeteners to the extent that they were forced to prematurely terminate the study because of the severity of reactions in patients with a history of depression (which is highly comorbid with anxiety).
For individuals who prefer not to eliminate sweeteners from their diet, options like stevia and erythritol could be viable choices. These are thought to have a negligible effect on insulin sensitivity and the microbiome, potentially reducing the risk of metabolic issues. However, it’s important to note that there is currently no conclusive data to support these claims.
Gluten proteins increase zonulin expression, the process by which zonulin (a protein that plays a crucial role in regulating the permeability of tight junctions in the lining of the digestive tract) is produced and released by the body’s cells.
As a result, compounds from digestion leak from the gut into the bloodstream (known as “leaky gut”), leading to inflammation. Zonulin has also been linked as a biomarker of mental illnesses from ADHD to schizophrenia.
It would seem logical then, that a gluten-free diet would aid in decreasing anxiety. While this was found to be the case in this study in celiac patients, there are not yet any studies that show the effects of a gluten-free diet on other cohorts, but hopefully, it is just a matter of time.
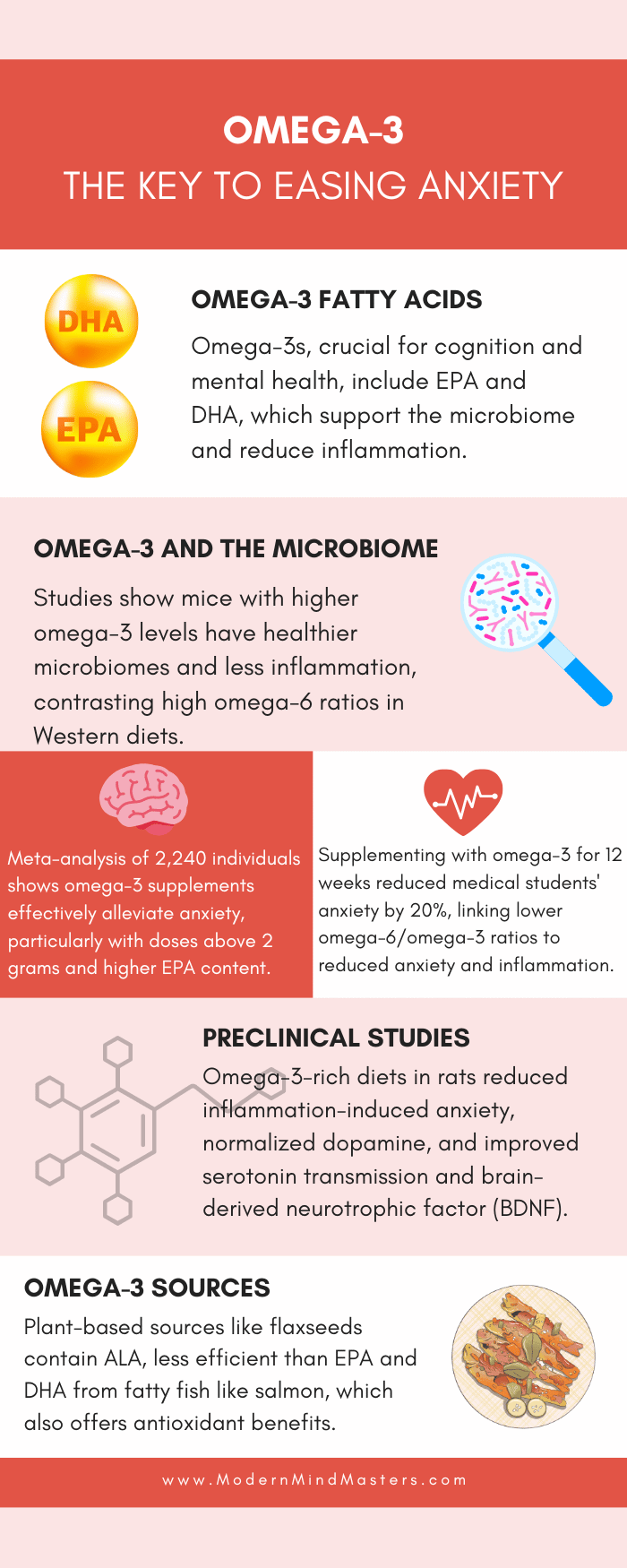
Omega-3 fatty acids are one of the holy grails of nutrition, so it is of little surprise that they have been found essential for cognition and mental health.
In particular, the long-chain omega-3s, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) are potent anti-inflammatory signaling molecules that support the microbiome.
This study found that on identical mice, those that biosynthesize omega-3s and have lower omega-6/omega-3 ratios exhibit healthier microbiomes, less inflammation, and less chronic disease. While omega-6 fatty acids are not inherently bad, health issues arise from a higher ratio of omega-6 to omega-3, as is common in Western diets high in processed foods.
Preclinical studies on rats suffering from inflammation-induced anxiety showed that omega-3-rich diets were able to normalize dopamine levels, reduce anxiety-like behaviors, and improve serotonergic neurotransmission and brain-derived neurotrophic factor (BDNF). Quite impressive!
Human trials have also yielded similarly promising results. This study found that in individuals with social anxiety disorder, the levels of EPA and DHA in red blood cells are decreased by 18-34%. Furthermore, they observed a reverse relationship between the concentrations of these omega-3 fatty acids and the intensity of anxiety symptoms.
In a study involving 68 medical students, taking omega-3 supplements for 12 weeks was found to reduce anxiety by 20%. The research also indicated that a lower ratio of omega-6 to omega-3 was associated with reduced anxiety levels and lower inflammatory markers.
Additionally, a comprehensive meta-analysis of nineteen clinical trials, encompassing 2,240 individuals from eleven countries, determined that omega-3 supplementation is an effective method for alleviating anxiety.
These investigations also emphasized the significance of both the dose and type of omega-3. Studies administering doses below 2 grams per day generally did not show effectiveness in alleviating anxiety.
Additionally, analysis of specific groups revealed that omega-3 supplements with a lower ratio of DHA were less effective in reducing anxiety. Supplements consisting of more than 60% EPA did not demonstrate a significant impact.
Plant-based omega-3 sources, like flax and chia seeds, mainly contain alpha-linolenic acid (ALA). This shorter-chain omega-3 converts into the more bioactive forms, EPA and DHA, but only at a very low efficiency, approximately 5%.
In contrast, fatty fish such as mackerel, sardines, and Alaskan sockeye salmon are much richer sources of EPA and DHA. Salmon is particularly notable for containing astaxanthin, an antioxidant that not only imparts a pink-red hue to the fish but also protects the omega-3 fatty acids from oxidation and offers neuroprotective benefits.
Curcumin, the main active ingredient found in the spice turmeric, is probably the most heavily studied spice for brain health, with dozens of studies noting its benefit in the treatment of Alzheimer’s and Parkinson’s disease, depression, and anxiety itself.
Mechanisms of action for curcumin include improving the gut microbial ecosystem, decreasing inflammation, and altering dopamine, serotonin, and cortisol levels. Quite the resume!
Preclinical trials of curcumin for anxiety in rodent models add to the promise of curcumin as an anxiolytic; in rats treated with a food preservative to induce anxiety, curcumin treatment completed alleviated anxiety-like behaviors.
In patients with diabetes, eight weeks of curcumin supplementation decreased anxiety, while a crossover trial on 30 obese individuals likewise found that curcumin supplementation for 30 days reduced anxiety scores.
Some critics argue that the acclaimed health benefits of turmeric and its active compounds, like curcumin, are exaggerated, arguing that despite showing promising results in laboratory tests, it may not be as beneficial in real-world applications.
Firstly, curcumin is chemically unstable, which might limit its effectiveness as a treatment. Secondly, curcumin has the potential to interfere with the laboratory tests (assays) themselves, which could lead to misleadingly positive results that don’t accurately reflect its true efficacy in treating health conditions.
Additionally, these skeptics highlight the significant inconsistency in research regarding the purity and composition of supplements used, complicating the ability to reliably replicate study results. For this reason, curcuminoids should be consumed with fats or black pepper, which aid in the absorption of curcumin by the body.
Combining curcumin with omega-3 has also been shown to have a cumulative benefit. Curcumin helps in converting ALA (a type of omega-3 fatty acid) into DHA by boosting the activity of enzymes responsible for this conversion, increasing the amount of DHA in the brain while also having a direct impact on reducing anxiety.
Vitamin D insufficiency, defined as levels below 30 ng/mL, is a widespread issue in the United States, affecting an estimated 77% of the population, and could potentially be considered a hormonal epidemic.
The modern lifestyle contributes significantly to this issue; most people spend a lot of their time indoors, wear full clothing, or live in areas with higher latitudes, all of which limit the body’s natural ability to produce vitamin D from sunlight.
As a result, it is often challenging to obtain sufficient vitamin D through diet alone. To reach the recommended 600 IU of vitamin D, for example, one would have to consume an impractical amount of five gallons of whole milk every day. This is even more daunting considering that some health practitioners advocate for higher daily intake than the standard recommendation.
In the brain, vitamin D regulates calcium homeostasis and ion channels, neurotransmitter levels, including dopamine and serotonin, and the secretion of nerve growth factor and BDNF. The benefits of vitamin D are also likely mediated by its role in shaping the microbiome and reducing inflammation.
Lower levels of vitamin D are associated with multiple mental disorders, including schizophrenia, depression, and anxiety. One study found that vitamin D levels in patients with a wide range of anxiety disorders were less than 60% of those of healthy controls.
In a study involving 30 individuals with anxiety, administering 50,000 IU of vitamin D once a week for three months led to a significant improvement in their symptoms. Another study, focusing on 51 women with type II diabetes, found that taking 50,000 IU of vitamin D every two weeks helped decrease inflammation and alleviate anxiety symptoms over four months.
Vitamin D supplements may be only beneficial for reducing anxiety in individuals who are deficient in vitamin D. Given that a significant portion of the United States population has some level of vitamin D deficiency, the overall impact of such supplementation is likely to be favorable.
Ketogenic diets – high-fat, low-carbohydrate diets that induce the body to produce ketones, a fuel source for the brain – are gaining traction as a metabolic treatment for a wide range of chronic metabolic diseases.
Having already been used for a century to treat some forms of epilepsy, they are now gaining in popularity for the treatment of neurodegenerative conditions, such as Parkinson’s and Alzheimer’s disease.
Similar to previous mechanisms, ketogenic diets have been found to address neurotransmitter imbalances, oxidative stress, and inflammation, all of which are known to affect anxiety.
Ketones, molecules created by the liver from fats when glucose is scarce, are not only a more efficient fuel substrate for the brain but also shift the gut microbiome and improve gut barrier function while reducing oxidative stress and inflammation.
This study on rats who were given ketone supplements to achieve ketone levels similar to those on ketogenic diets exhibited significant decreases in anxiety.
There is also evidence that intermittent fasting, an intervention that induces ketosis, induces neurological adaptations over time that are neuroprotective and reduce anxiety.
While clinical trials assessing the efficacy of ketogenic diets for anxiety in humans are yet to be conducted, they present a potentially promising future for nutrition and mental health.
While conventional medications and therapies maintain their importance, the burgeoning field of metabolic medicine and nutritional psychiatry offers a complementary and promising avenue.
It’s clear that our diet – what we consume and how it affects our gut microbiome, inflammation levels, and brain function – plays a critical role in managing and potentially alleviating anxiety.
From the impact of omega-3 fatty acids in balancing our inflammatory response to the intriguing benefits of curcumin in modulating neurotransmitter levels and gut health, the evidence points towards a more holistic approach to treating anxiety.
The potential of vitamin D supplementation and ketogenic diets further illustrates the profound connection between our dietary choices and mental well-being. However, it’s essential to recognize the individual variability in response to these nutritional strategies, emphasizing the need for personalized approaches in treating anxiety.
As we unravel the complex interactions between diet, the microbiome, and brain health, it becomes increasingly evident that what we eat goes beyond mere physical nourishment. It’s a powerful tool in our arsenal for mental health, offering a pathway to manage anxiety with fewer side effects and more attuned to the unique needs of each individual.
While we await more comprehensive human trials and deeper understanding, the existing evidence opens up exciting possibilities for integrating nutrition into our overall strategy for mental health care, offering hope and new solutions for those struggling with anxiety.
Diet significantly impacts anxiety by influencing the gut microbiome and inflammation levels in the body. For example, artificial sweeteners can exacerbate anxiety while omega-3, curcumin, and vitamin D has been shown to alleviate it.
Nutritional psychiatry research shows that foods rich in omega-3 fatty acids, for instance, can reduce inflammation and balance brain chemistry, while artificial sweeteners have been shown to increase brain inflammation.
Imbalances in gut bacteria can affect the brain via the Vagus nerves which influences hormonal regulation, increase inflammation, and disrupt neurotransmitter balance, all of which can increase anxiety levels.
The brain needs many foods for success; a lack of any one of the hundreds of nutrients will result in poor cognitive health and performance.

They are many reasons why you may be struggling to sleep, including genetic and environmental reasons. Here are the most common problems and how to overcome them.
Too much dopamine can be a bad thing; overindulgence will lead to lower motivation, addiction, and even depression. Learn how to dopamine detox with these 5 activities
Knowledge is not power without action, and habits form the consistent actions that compound over time to guarantee success.
Ketamine, through ketamine therapy, has been shown in clinical settings to benefit mental health, specifically depression and other mood disorders.

Follow these 7 simple steps that work alongside your body to learn how to stop oversleeping.
© 2025 Modern Mind Masters - All Rights Reserved
You’ll Learn:
Effective Immediately: 5 Powerful Changes Now, To Improve Your Life Tomorrow.
Click the purple button and we’ll email you your free copy.