The Subconscious Mind – What Is A Subconscious?
The subconscious mind has long been surrounded by mystery, but cognitive sciences are unravelling the mystery.
Serotonin syndrome has loomed over humanity for centuries. Once known as “convulsive ergotism” from overdosing on serotonergic plants such as St. John’s wort in medieval Europe, today we link it to advanced medications such as antidepressants.
The condition, resulting from an excess of serotonin—a key neurotransmitter in mood, digestion, and sleep—illustrates the paradox of pharmacological interventions. As antidepressants, particularly Selective Serotonin Reuptake Inhibitors (SSRIs), become more widespread, so does the incidence of serotonin syndrome, walking a fine line between therapeutic effect and toxicity.
This article ventures into the heart of serotonin syndrome, uncovering its roots from drug-induced serotonin surges to the chaotic effects of certain supplements and recreational drugs.
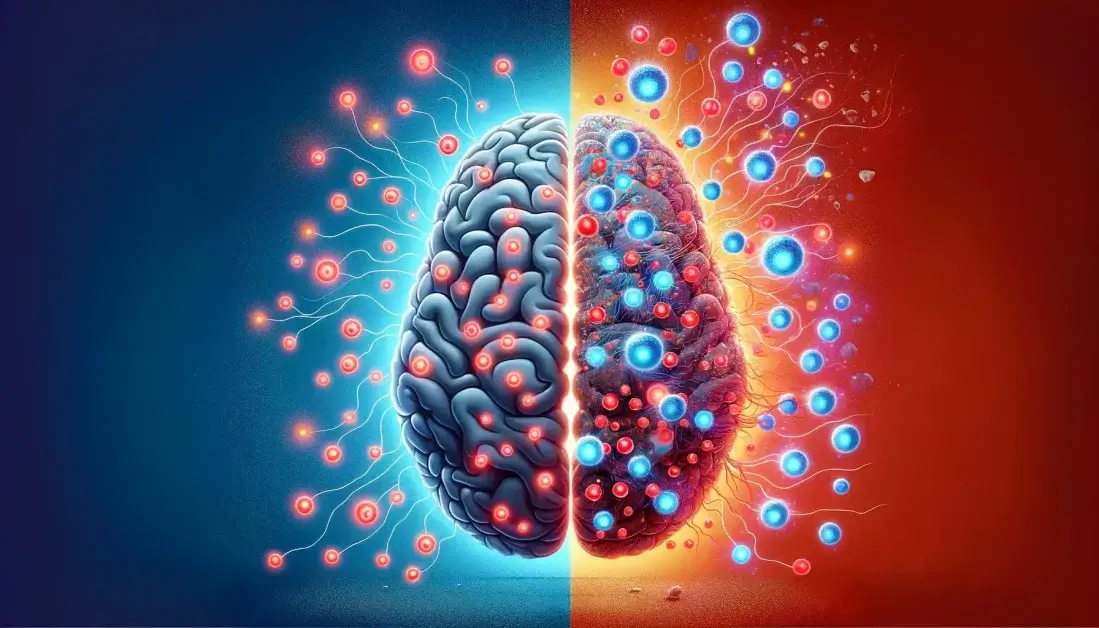
Serotonin is a neurotransmitter that plays a crucial role in mood regulation, digestion, sleep, and other bodily functions. Certain drugs and compounds, namely antidepressants such as selective serotonin reuptake inhibitors (SSRIs), can elevate serotonin to harmfully high levels.
Such dangerously high levels of serotonin in the brain is known as serotonin syndrome, also referred to as serotonin toxicity. While the effects are often mild, it is a potentially life-threatening condition.
Drugs and compounds that elevate serotonin increase serotonergic activity in both the peripheral (PNS) and central nervous systems (CNS) and are characterized by clinical findings of high free serotonin (5-HT) or 5-HT receptor activation within the brain.
There is no confirmatory test or specific laboratory findings that can categorically diagnose serotonin syndrome, and the syndrome has a broad spectrum of severity ranging from barely perceptible to lethal.
Serotonin syndrome occurs in all age groups, and the incidence is rising alongside the increased use of serotonergic agents.

Serotonin syndrome is most commonly the consequence of therapeutic medication use, interactions between medications or recreational drugs, or intentional overdose.
Drugs of abuse, such as cocaine, MDMA, and other amphetamines, cause increased release of 5-HT (the chemical name for serotonin), effectively flooding the brain with serotonin.
Dietary supplements, such as tryptophan (the precursor of serotonin), increase the rate of 5-HT synthesis, where the body produces more serotonin from its biological precursor, tryptophan.
Prescription antidepressants, such as Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Tricyclic Antidepressants (TCAs), and Dopamine-Norepinephrine Reuptake Inhibitors (DNRIs), all work by the inhibition of 5-HT uptake from the synaptic cleft.
By inhibiting the reuptake of serotonin, these medications increase the space between neurons where neurotransmitters are released and bind to receptors on the postsynaptic neuron. If too much serotonin is inhibited, however, serotonin syndrome can result.
Several medications can trigger serotonin toxicity through different mechanisms.
Selective Serotonin Reuptake Inhibitors (SSRIs) like citalopram, escitalopram, fluoxetine, paroxetine, and sertraline work by stopping serotonin from being reabsorbed back into the presynaptic neuron from the synaptic cleft. This process increases the level of serotonin available in the brain.
A range of other medications also block the reuptake of serotonin, including pain relievers like meperidine and tramadol; medications such as pentazocine, metoclopramide, valproate, carbamazepine; the cough suppressant dextromethorphan; and the muscle relaxant cyclobenzaprine.
Drugs known as serotonin modulators, for example, trazodone, and dopamine-norepinephrine reuptake inhibitors like bupropion, enhance the availability of serotonin in the synaptic cleft. Tricyclic antidepressants and St. John’s wort, a commonly used supplement, similarly prevent serotonin reuptake.
Serotonin Syndrome (SS) is typically caused by starting two or more drugs that increase serotonin at the same time. However, the syndrome can also arise from beginning just one serotonergic drug in sensitive individuals, adding another serotonergic drug to a regimen that already includes one, or from an overdose of such drugs.
It’s particularly risky to combine a monoamine oxidase inhibitor (MAOI), especially MAO-A inhibitors that specifically target the breakdown of serotonin, with drugs that increase serotonin levels. This combination can lead to a very severe form of serotonin syndrome and, in some cases, even death.
The difficulty of diagnosing serotonin syndrome means the true incidence is unknown. Mild cases are frequently overlooked or dismissed, while more serious cases are commonly attributed to other causes.
Serotonin syndrome is a condition that is not commonly encountered and may not be readily identified in randomized clinical control trials. This condition tends to be under-recognized and under-reported by healthcare professionals, with one survey revealing that 85% of general practitioners (GPs) were unfamiliar with the condition. Furthermore, mild cases of serotonin syndrome are often overlooked or resolved on their own without medical intervention.
It is likely, however, that the prevalence of serotonin syndrome is increasing alongside the rise of adults taking antidepressants. In the United States, the rate almost doubled from 6% to 10.4% between 1999 and 2010.
The wide range of possible symptoms further adds to the difficulty in identifying and diagnosing it.
Symptoms of serotonin syndrome can vary widely, from very mild to extremely serious. They often involve changes in mental state, issues with body regulation, and overly active muscles. This can mean anything from slight shakes that are hardly noticeable to dangerous increases in body temperature and severe reactions.
Common signs include feeling agitated, anxious, restless, confused, sweating a lot, having a high fever, fast heart rate, feeling sick, shaking, stiff muscles, quick reflexes, jerking movements, wide pupils, eye twitching, dry mouth, red skin, and loud stomach noises.
Sometimes, mild symptoms like shaking or restlessness might be missed or thought to be anxiety or another mental health issue. If there are stomach problems, people might think it’s just a stomach bug or bad food.
Unfortunately, there is no laboratory test or empirical measure that can confirm a diagnosis of serotonin syndrome. Instead, doctors must look for several criteria for making a clinical diagnosis. The Hunter criteria, however, are generally accepted as the most accurate.
Hunter Criteria
While the Hunter test is generally accepted as the most accurate, the criteria were designed specifically for patients with SSRI overdose, not serotonin syndrome from other agents; therefore, it may not reveal the disease in patients with minor symptoms.
As always, seek advice from a qualified professional regarding serotonin and serotonin syndrome.
Serotonin syndrome typically resolves itself within 24 to 72 hours without any long-term effects if it’s caught early and treated by stopping the drug that caused it and providing the right supportive care.
The symptoms usually appear quickly after taking the drug that triggers the syndrome: about 30% of people will notice symptoms within an hour, 60% within six hours, and almost everyone who’s going to react will see symptoms within the first 24 hours after taking the drug.
If someone hasn’t shown any symptoms 6 to 8 hours after taking too much of a drug, they’re probably not going to have a severe reaction.
SSRIs are not often linked to death, even if taken in large amounts unless taken with other drugs. Deaths that do happen are usually within the first 24 hours after taking the drug and are more common with another type of medication called MAOIs than with SSRIs.
Treatment for serotonin syndrome primarily involves immediate action to address the condition, focusing on stopping the use of medications that increase serotonin levels, ensuring proper hydration, and providing supportive care.
This supportive care is critical for managing symptoms such as high blood pressure, elevated body temperature (hyperpyrexia), and potential respiratory or cardiac complications that may arise.
In most instances, serotonin syndrome is mild and can be resolved simply by discontinuing the drug responsible for the condition. Once all serotonergic medications are stopped, the management approach shifts to supportive care, emphasizing the prevention of complications that could arise from the syndrome.
This includes close monitoring of vital signs, administering fluids to maintain hydration, and using medications to control specific symptoms, such as antihypertensives for high blood pressure or cooling measures for fever.
The goal is to support the body’s systems while the effects of excess serotonin dissipate, ensuring a safe recovery from the syndrome.
Serotonin syndrome is a critical reminder of the complex interplay between pharmaceuticals and our body’s delicate biochemical balance and is a result of therapeutic drug use, drug interactions, and occasionally, recreational drug abuse or dietary supplements.
The increasing prevalence of serotonin syndrome, alongside the rising use of antidepressants and other serotonergic agents, demands a heightened vigilance for its symptoms—a range spanning from subtle to life-threatening.
The absence of a definitive test for SS necessitates a reliance on clinical diagnosis, primarily the Hunter Criteria, emphasizing the importance of medical professionals being well-versed in recognizing the signs of this syndrome.
Treatment focuses on cessation of serotonergic drugs and supportive care, which, if promptly initiated, typically leads to resolution within 24 to 72 hours, highlighting the potential for full recovery with appropriate intervention.
In essence, serotonin syndrome encapsulates the paradox of modern medicine: a testament to our progress, yet a cautionary tale of the fine balance we must navigate between healing and harm.
Serotonin syndrome is a condition caused by excessive serotonin levels in the brain, triggered by serotonergic drugs, supplements, or interactions, leading to a range of symptoms from mild shakes to life-threatening conditions.
Serotonin syndrome symptoms include agitation, confusion, high fever, fast heart rate, muscle stiffness, jerking movements, wide pupils, and gastrointestinal issues.
Serotonin syndrome typically resolves itself within 24 to 72 hours without any long-term effects if it’s caught early and treated by stopping the drug that caused it and providing the right supportive care.
The subconscious mind has long been surrounded by mystery, but cognitive sciences are unravelling the mystery.

Reverse osmosis water filter systems are the gold standard in water filtration, effectively removing a wide range of contaminants and disinfectant byproducts.

While social media can be a powerful tool, many end up abusing it to the detriment of their mental health, contributing to depression, anxiety and addiction.

Procrastination may seem illogical, but there are strong biological reasons behind it. These tips will show you how to stop procrastinating for good.
To master emotions, and improve emotional control, we first need to understand the science behind them.
Too much dopamine can be a bad thing; overindulgence will lead to lower motivation, addiction, and even depression. Learn how to dopamine detox with these 5 activities
© 2025 Modern Mind Masters - All Rights Reserved
You’ll Learn:
Effective Immediately: 5 Powerful Changes Now, To Improve Your Life Tomorrow.
Click the purple button and we’ll email you your free copy.